Our latest Patients Have Power episode is called "I cannot afford to go back." (You can subscribe to the podcast at Apple Podcasts, or listen to it with the media player above).
In this episode, I'm joined by Aaron, Clara's Head of Growth, to chat about the various impacts disease can have on a patient's financial stability and how we can come together to share resources, beat stigma, and help improve the healthcare landscape for all patients.
Below is a transcript of the episode for your reading pleasure!

Lilly Stairs: Hello, everyone. Welcome to the Patients Have Power podcast. We are mixing it up a little bit this week, and now, every other week. I have Aaron Jun with us. He is Clara's Head of Growth. Aaron, welcome.
Aaron Jun: Thanks for having me.
Lilly Stairs: Well, I guess now we're sharing the podcast a little bit. You're stealing my thunder.
Aaron Jun: A little bit, and I apologize for that. But hi, everyone, this is Aaron. I work closely with Lilly, and basically what I do is I try to help tell a lot of these patient stories that we hear, try to craft the message a little bit. But it's fantastic to finally join this podcast that I help edit every single week.
Lilly Stairs: I have no tech abilities whatsoever.
Aaron Jun: I just wanted to be a part of it, and this is a good excuse. I think every other week we'll be bringing some stories. Not necessarily patient stories, but stories and current events happening around health, health tech, patients, and health care.
Lilly Stairs: Yeah, because we've really been blown away. Granted, I'm a patient, so I've seen a lot of this, but oh my God, my eyes have been opened to a whole nother world of what patients go through each and every day. We think it's so important to start highlighting these issues and bring them to the forefront so that we can hopefully open up conversations and dialogue that's going to effect change.
Aaron Jun: Yeah, and I think that the word "conversation" is probably the key here. I don't think Lilly and I are going to solve any of the big things just by ourselves, although we have some ideas. But what we really want is, like you said, to start the conversation or to have some conversation and maybe spark some interest with our audience.
Lilly Stairs: Yeah. This week, we thought the first topic that we definitely had to hit on was the economic burden that patients are facing when they are living with a chronic illness. It is mind-boggling. It's scary, quite frankly, what we hear.
Aaron Jun: Yeah. Lilly, we'll get into your personal story at some point during this conversation, I'm sure, but it is something ... I'm a relatively healthy guy, and-
Lilly Stairs: Relatively. He's got some-
Aaron Jun: Relatively.
Lilly Stairs: ... back issues that he complains about almost every day.
Aaron Jun: The back issues are troubling, but Advil fixes most of it. I'm sure if I stretched, it would solve almost all of it.
Aaron Jun: I think at a high level, everyone understands that being sick can be very expensive, but I don't think a lot of us, especially those are us who are blessed with decent health, understand just how crippling not just the disease is physically, but also economically.
To that point, we had a story come in from one of the patients that we've worked with and I just wanted to read it and begin the discussion that way if that's okay.
Aaron Jun: This is from a patient, and she says:
"My husband died of a rare disease on November 11, 2016, leaving me in a huge financial hole. Six months later, I developed my own rare disease after shingles ravaged my nervous system." It's central pain syndrome, is what she had.
After working for 15 years as a nurse, I slowly lost everything. My health, my home, every cent of savings, and retirement that I had saved. Next, I fought for disability, was denied twice, paid a lawyer almost half of my back disability pay when it was approved on the third try.
The system is dreadfully broken. If I didn't have family and friends to fall back on and help lift me up again, I can't imagine where I'd be. I thought I was fairly well prepared for crises in my life. Instead, I'm the example of what can happen to a hard-working professional with insurance, a home, savings, and retirement accounts. I hit rock bottom fast. Sadly, anyone can. Over a decade later, I'm still fighting my way back."
Aaron Jun: Sadly, what we find here at Clara, anyway, is that this is not an uncommon story. Many of the patients who come through Clara ... What we do at Clara is match patients to clinical trials. Many of these patients who come through are coming not because they necessary want to take part in a clinical trial, but because they have been denied by insurance, or dropped by insurance, or are facing any sort of financial hardship.
Aaron Jun: This story sounds very extreme when you read it out like this, but it's actually a very common thing in the American health care system and everyday American life.
Lilly Stairs: It's scary, and one thing I do wanna say because she did give us permission, this was Becky Brandt.

She's one of our Breakthrough Crew ambassadors and she said, "It's really important to me that people are able to put a face to the story." I wanted to make sure that we gave her a shout out, there, and I appreciate, Becky, your bravery, your honesty, for sharing with us.
Aaron Jun: Definitely.
Lilly Stairs: You can follow Becky @bbhomebody on Twitter. She also is the co-founder of an awesome nonprofit organization and does a lot of work around central pain syndrome. Anyways, I just wanted to get that in to make sure we put that face to the name.
$5,800
Lilly Stairs: But it is, it's absolutely scary, and we're seeing a lot of patients ... We know chronic illness patients, how critical it is to have a specific treatment plan. We're all different. We all respond very differently to medications, and for some reason, insurance companies don't understand that.
Aaron Jun: We are trying to be delicate, here, because obviously insurance companies and pharmaceutical companies, everyone has their own incentive structures. It can't be all free for everyone all the time forever, so there is an element of understanding there.
Aaron Jun: But having worked with Lilly, now, for a little over a year, and having had many glasses of wine with her, and having had many breakfast sandwiches with her, I've come to understand-
Lilly Stairs: No sandwiches. I don't really eat the bread.
Aaron Jun: Right. Well, and we can talk about that.
Aaron Jun: And having heard so much about her own health journey, it is shocking that there is so much hurdling that is required from the patients as they're going through some of the worst times of their lives to also follow up with insurance companies, and make these calls over and over again, and demand some payment or some justice. It's just absolutely mind-boggling just how many hurdles and hoops are set up along the way to treatment.
Aaron Jun: 'Cause treatment sounds so easy. It's like, "Oh, it's just get diagnosed and get treated." But even that is pretty harrowing and difficult in and of itself to get the treatment.
Lilly Stairs: Absolutely.
Aaron Jun: And, Lilly, I hope you don't mind if I share this bit, but ...
Lilly Stairs: I don't know where you're going.
Aaron Jun: No, it's nothing personal.
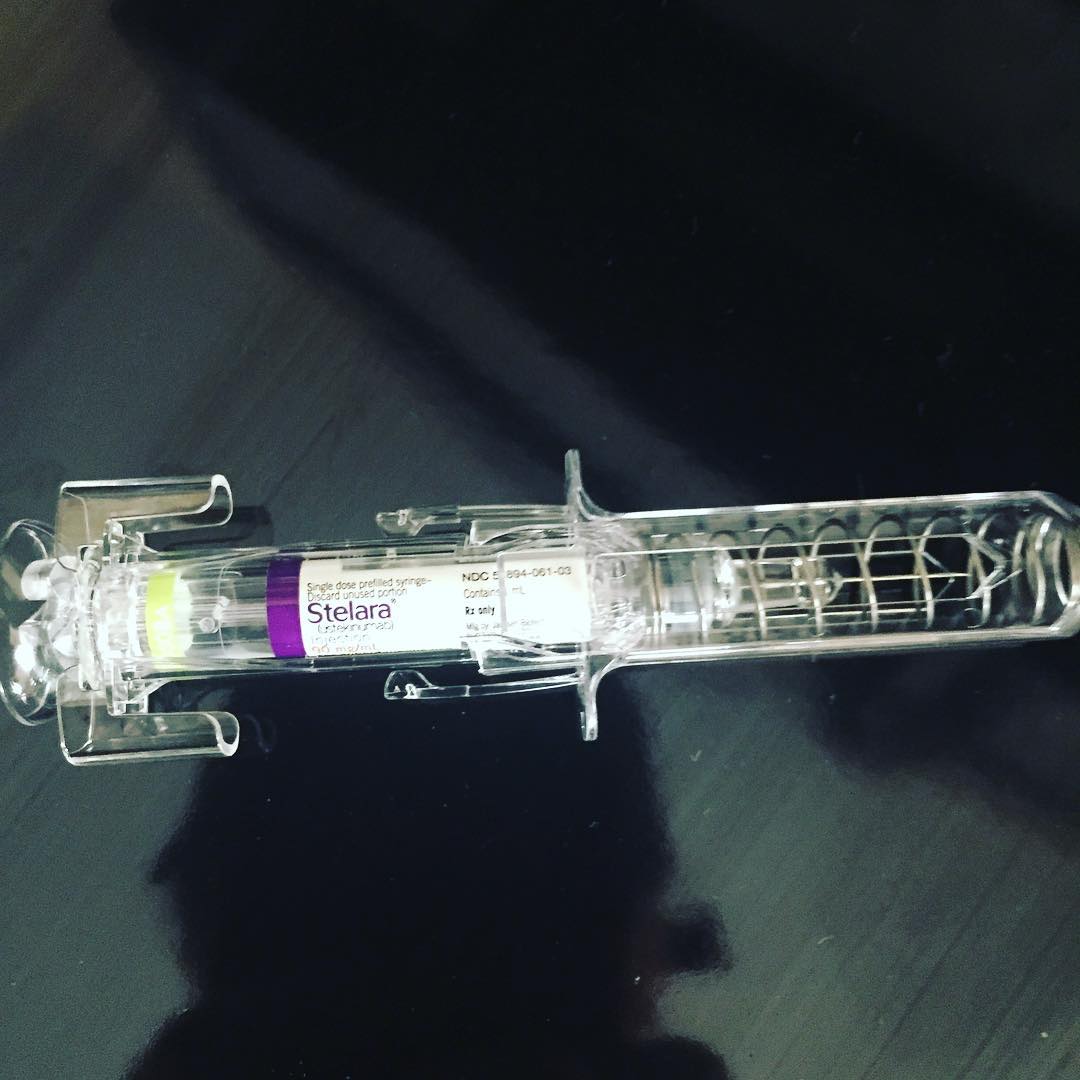
Aaron Jun: Lilly has a few autoimmune conditions, and thankfully, she's in remission. One of the things that helps keep her in remission is her biologic. For a year's worth of this biologic, it's $120,000, which thankfully is covered under insurance today.
Lilly Stairs: Insurance and a pharmaceutical patient assistance program.
Aaron Jun: Okay, right.
Lilly Stairs: It's really wonderful. A shot that is typically around $20,000 actually only costs me five dollars every two months, which is remarkable. I'm very fortunate to be in that situation.
Aaron Jun: But we are going on to a company health care plan, and in the search for this, it's become clear to us that, just because we pick the Cadillac plan, just because we pick the gold-plated one that's supposed to be the best, doesn't necessarily mean that this biologic even gets covered.
Lilly Stairs: No, it doesn't, and I've been afraid. Every day I've really been thinking about this proactively in the process of trying to figure out health insurance. I'm on a health insurance plan right now where I've been very fortunate in that most of the therapies that my physician has wanted to put me on has been covered.
Lilly Stairs: I tried and failed several biologics, which is the story of most autoimmune patients' lives. I am fortunate to be on one that has put me into remission, but that doesn't mean when we switch to this next insurer that they're gonna cover my specific medication.
Because what's happening is that a lot of these insurance companies are looking at biologics as a class, and they're not really differentiating between the fact that there are different mechanisms of action within these different biologics.
Lilly Stairs: There's only one specific mechanism of action that works for me, but maybe they've cut a deal with a pharma company so they have a preferred biologic that they want someone to use.
I cannot afford to go back and have to go try these biologics again, go through a step therapy process to get back onto the drug that makes me healthy, because the fact of the matter is, without this medicine, I don't move.
Lilly Stairs: I've have total body arthritis, we've talked about this. I'm lying in bed. I can't even dress myself. I have bleeding ulcers in my small intestine. I am effectively just bedridden.
Aaron Jun: Right, and the thing that blew my mind this morning as we were talking over coffee was the idea that you would have to go back onto step therapy potentially. Which it sounds like absolute madness, but because insurance doesn't necessarily carry over from Massachusetts where we were just a few weeks ago to California where we are now.
There might be the same hurdles and hoops that we need to hop through on your behalf, or that you need to hop through to get back to where you were, which is just absolutely wild to me.
Lilly Stairs: Yeah, and this is the case for ... We've got, what is it, about 50 million Americans who are living with some type of autoimmune disease and then we see so many of them coming in through Clara all the time.
Lilly Stairs: They're all trying to manage this in some capacity. Some don't have insurance, some who have had insurance and been stable on their medicine for a long time but then all of a sudden their insurance switches their formulary and they can no longer afford it ...
Lilly Stairs: Is this what we've come to? That people like Becky, who worked so hard their entire lives, have everything taken away from them because they drew the short straw? That they're now sick? How is that fair?
Aaron Jun: It's absolute madness, and the thing that, again, boggles my mind ... I honestly can't think of many other ways to say it, but it is mind-blowing and mind-boggling.
Aaron Jun: Lilly, you and I have worked together, now, for a year, and I can't imagine where this company would've been without having you around to help guide the voice and help guide how we approach patients. The idea that someone like you, or someone like Becky, or anyone, really, is at the mercy of health insurance to this extent is absolutely crazy to me.
Lilly Stairs: Yeah. It is, and this is just one component. We have the medicine, but then we also see there are a lot of patients who are addressing their diseases through other methods.
Lilly Stairs: So, some integrated medicine. We're looking at diet, we're looking at lifestyle changes. Again, that's actually not something that's traditionally covered by insurance, but it's something that many patients are forced into whether they like it or not.
Aaron Jun: Right. You bought ... Remind me how expensive the loaf of sourdough was that you bought.
Lilly Stairs: Okay, so it was really good. For context, here, we just moved to California. Sourdough bread is really popular in California. What's the name of the place? Is it Boudin Bread?
Aaron Jun: Boudin.
Lilly Stairs: Boudin. I don't know.
Aaron Jun: Boudin. I took Spanish.
Lilly Stairs: But there's these bread bowls, and I'm like, "Oh, God, this looks so delicious." I've been gluten, dairy and soy free for a number of years, now; I've found that it helps keep my autoimmune diseases in check. I've tried to go and cheat and I just don't feel well when I do that.
Lilly Stairs: I was really excited, though, because we have so many options here, in California, for people who are anything free. Vegan, gluten, dairy, soy, sugar. Tons of stuff. But I did splurge and get a $10 little, tiny loaf of bread.
Aaron Jun: Do you remember how big it was? You just made the smallest motion with your hands.
Lilly Stairs: I don't know. Maybe ...
Aaron Jun: It's not a baguette. It's not a long baguette thing.
Lilly Stairs: It's not a baguette. It's maybe a quarter of the size of a baguette, but you know what? I didn't even care because I was like, "Finally I can eat something. This is this normal thing that everybody else gets to eat." Everybody gets to eat the sourdough bread when they come to San Francisco, but I was in this place where I couldn't.
Lilly Stairs: Finally people have started making that, and that's awesome, but it also costs two, three, four times the amount that the average person pays. My grocery bills, that applies across the board to everything. If one-
Aaron Jun: Right, because you have to buy organic.
Lilly Stairs: Again, everything is twice as much. Two to three times as much. I don't know. Pasta. How much is a box of pasta for a normal person?

Aaron Jun: The cheapest one's probably 79 cents.
Lilly Stairs: Okay. I pay between $2.50 to $3.50 a box for a box of gluten-free pasta.
Aaron Jun: I'm just trying to imagine. What if you had a family, and what if you had a child, or what if you and your child were both having to live by this diet and nothing got covered?
Lilly Stairs: I don't know. How do I afford that? And it's not just the food. It's this combination of the food, the medicine, the lifestyle. There are certain accommodations I need to make.
Lilly Stairs: We were talking earlier today about public transportation. When you're in a flare and you're not feeling well, you don't really wanna take the risk of getting on public transportation and not having a seat. Especially when you have an invisible illness and nobody can tell.
Lilly Stairs: I'm this young 20-something and I go try to take a seat, but then an elderly person comes up and everyone's looking at the young 20-something like, "Get up so that this elderly person can sit down."
It's like, "Well, you don't know that I actually am in so much pain. This elderly person probably has a healthier body than I do." Now I'm adding taxis, or Ubers, or Lyfts, or whatever it might be to my list of expenses, because I don't feel well enough to take public transit or walk.
Aaron Jun: You just wanna be ensured that you can sit down for 20, 30, 40 minutes.
Lilly Stairs: Yeah. These are all the things that I ... We are scratching the surface, here, of expenses that patients incur. We're not even really digging down deep. There are so many, and it's just something that we need to keep in mind for those of us who are working in health care. What can we do to ease this burden on patients? I don't have the answer.
Aaron Jun: Neither do I. Hopefully someone listening out there has some better ideas or have seen ideas work somewhere else. Right now, things are ...
Aaron Jun: I think over the last year, seeing the ACA come back into the news so frequently, I was reminded that even simple health care or even the most lackluster or bare-bones access to insurance is a premium to most Americans. The idea that we are, right now, looking at pretty much some of the best health care plans in California and we still don't have assurances that Lilly's gonna be covered ...
We're not doing this for me. We're doing this for Lilly and for whoever else we might hire who has these considerations to make. They have no assurances that they won't have to be going through some crazy process to get to the medicine that they need.
Aaron Jun: It's absolutely stunning to me, and I wish that the system was a little more ... we say this all the time, but patient-centric.
Lilly Stairs: The industry's favorite buzzword.
Aaron Jun: Right, it's such a buzzword. How many conventions have you been to or have we sent you to where patient centricity was the talking point of the hour, of the day, of the evening, and you were the only patient in the room?
Lilly Stairs: Oh, it's painful. It's painful. Jen, from Savvy Coop, called this out when she went to JPM. It's just like,
"Where are the patients? Where are they?"
And I was just at a conference, and every single person gets up on stage and they're like, "You need to do things in partnership with patients," but there's not a patient up on stage presenting with them.
Lilly Stairs: I don't understand this mentality. So much of it is for show right now. There are some companies who are truly doing it and truly working with patients, and I believe that those are the companies that will be successful in disrupting the system. But not enough people are doing it.
Aaron Jun: No, certainly not. I do think health care having such entrenched players for so long probably have ... They might be trying their best, but they might just be slow moving. Whatever the case is, it's just not good enough.
Lilly Stairs: No.
Aaron Jun: We need a lot better, and hopefully, with enough people starting that conversation ... I won't pretend this is any major conversation that's gonna get on CNN or anything, but by having a lot of people start small conversations everywhere, hopefully we can crescendo it and arrive at a place where we really are having meaningful conversations in the rooms and in the hallways where they need to be happening for meaningful change to be enacted.
Right?
Lilly Stairs: Yeah, absolutely.
Aaron Jun: Yeah, and I'm looking at this AARDA Cost Burden of Autoimmune Disease report that you're sending around, Lilly, and-
Lilly Stairs: Let's take a step back and say what AARDA is.
Aaron Jun: Yes, sorry.
Lilly Stairs: AARDA is the American Autoimmune Related Diseases Association working to help bridge the gap and connect all the different autoimmune diseases. There's over 100 of them but we look at them all individually. So, AARDA's a nonprofit organization that's working to bring awareness on that front.
Lilly Stairs: Just wanted to make sure that we weren't throwing any weird acronyms at you without explaining. You go ahead. You can finish your thought.
Aaron Jun: We share these acronyms so often every single day that I just ... I apologize. But thanks for catching me on that.
Lilly Stairs: Always.
Aaron Jun: The estimated annual cost for autoimmune disease treatment was greater than $100 billion. This was back in 2001.
Lilly Stairs: And that's billion with a B.
Aaron Jun: That's billion with a B, right. Then there's this New York Times article that we were sharing around the office the other day where they were interviewing ... Everyone should read it. We'll link to it when we release the podcast.
Aaron Jun: But the price they pay, it was a New York Times investigative piece about the cost. Again, the economic burden of disease. They interview this woman in Wisconsin, and she says,
"I didn't cry when I was handed the diagnosis of MS, but after learning how much prescripts would cost, that's when I felt truly helpless."
Aaron Jun: She's a former journalist. She had coverage through her husband's employer and she had to take that coverage once she was no longer able to work. They hit their $4,500 annual deductible within the very first month of every single year that she's been on the drug that works for her because the drug, itself, carries a $5,500-a-month price tag, which is stunning to me.
Aaron Jun: I actually have a friend back in Boston who has colitis, and he's been on ... I can't remember the name of the drug. But his employer was about to switch insurance coverage, and he was no longer going to be covered. But unfortunately, he was not in a position high enough to push back against this insurance change, so he just had to take the brunt of it. Now he's working through it.
Aaron Jun: Again, watching that happen to a friend of mine, and reading these stories and imagining that it's Lilly, or my friend back in Boston, or anyone that I've met who's ever been sick ... It's appalling that this is such a heavy consideration that's an everyday reality for so many people in America. It's absolutely appalling.
Lilly Stairs: It is. What do we do? We're in this situation where it's not gonna change overnight. It's gonna take a lot to make waves and make changes.
Lilly Stairs: First thing's first. I think here at Clara we're really working to try to put together ... We're working alongside some of our Breakthrough Crew ambassadors to put together financial resources and other resources for patients to turn to.
Aaron Jun: Right.
Lilly Stairs: That's something that we'll share around as well is some of these financial resources we've started putting together, because we have some incredible advocates who have had to navigate the system. They've done it before and they wanna share their knowledge.
Lilly Stairs: There's a piece we're releasing from Allison, who is this amazing advocate. She has a few different autoimmune diseases, and she came to us with a list, this laundry list of resources, that she's uncovered over the years. We wanna help distribute that so that people have access to this. It's not gonna change everything.
It's not gonna fix everything, but at least it's a starting point.
Lilly Stairs: And what else can people do? What else can people do?
Aaron Jun: On the resources front, I think there are so many resources. You were just telling me one about the biologic that you're on today. The pharmaceutical who makes that, there is a program that they offer.
Lilly Stairs: Yeah, it's amazing. This is actually a really good example of something that, honestly, I had no idea. I work in health care. We're in this every single day.
We're talking about clinical trials, I'm looking at new treatments. I don't even know that this program exists for my own drug. I consider myself a really empowered patient, but I didn't even know about this.
Lilly Stairs: Basically, I'm an insurance plan now. I've been really stable on this drug for about four years, now; it's put me in remission. I spoke to some navigators at the company and I was like:
Listen, I'm really concerned. We're switching insurance. What's gonna happen? What if I lose this drug? Do you know which payers have been good about covering the drug?
Lilly Stairs: They're like, "Calm down. It's okay." They were actually really helpful. They were like, "You need to go meditate." I'm like, "Yeah, I know." They said that there is actually this program where, as long as you're on insurance ...
Lilly Stairs: The new insurance says, "Okay, no, we're not gonna cover the biologic." This pharma company that makes the biologic has a link program where, as long as I still have some sort of insurance, they'll give me that drug for free so that I have access to the drug and I can maintain my therapy, which is remarkable.
Aaron Jun: Which is amazing, and you had no idea, and neither did we.
Lilly Stairs: No friggin' idea.
Aaron Jun: And again, like you said, we work in this stuff. This is our-
Lilly Stairs: All day.
Aaron Jun: ... ideally 9:00 to 5:00, but it's generally longer hours than that. That's fine; we're happy to do it. But the point being, we spend hours a day just staring at this stuff and there's an ocean of material that we continue to uncover every single day.
I think one step that we can all take together as patient communities is to band together and share these resources as openly as possible.
Aaron Jun: I do think that a part of this is the problem of stigmatizing poverty. Maybe not necessarily poverty, but even being a little bit poor or middle-class.
I think the American culture stigmatizes that just a little bit, and I think we need to be very cognizant of the fact that there is no shame in being sick and having your economics get drained because you're sick.
Aaron Jun: Maybe in the past people didn't want to raise their hands and say, "Hey, this is literally bleeding my bank account dry."
But I think the more and more people that raise their hands and say, "This has been my experience. This thing helped. I went down this dead end, and this dead end, and this dead end. Do not go there," I think that'll be a good first step.
Lilly Stairs: Yeah, because we can sit here all we want, and we all have our own experiences, but the people who have lived it, the people who have been through it, they're the ones who have had to navigate it and find the hacks to get there.
Aaron Jun: The hacks.
Lilly Stairs: The patient hacks. The more that we can all elevate this message and talk about it together, that's gonna be so important. We share resources like this. We ban together to do that, and so I think that that's important. We will continue to do that.
If you have any recommendations, please send them our way. We're happy to help be your microphone and get these resources out to fellow patients.
Lilly Stairs: I think that we've covered a lot in this first podcast. I'm a little overwhelmed by everything we've covered in this short amount of time.
Aaron Jun: Yeah. I hope this didn't seem very doomsday. I do think that things will begin to change for the better.
Lilly Stairs: Yeah.
Aaron Jun: I think that there is this idea that, in the day to day, when we're all just seeing some of the bad news or hearing bad news from our friends, it can seem very overwhelming and like there's never gonna be a straw that breaks the camel's back.
Aaron Jun: But eventually, there is a straw that breaks the camel's back, and we just need to do everything we can as communities and health care and patient advocacy across the board in health care, health tech, to make sure that we are contributing what we can and to share our stories and to share our resources and to make sure that we're all just being as open as possible about things. Eventually, hopefully, things begin to look very different for everyone.
Lilly Stairs: Absolutely. Absolutely. I think that's really a beautiful sentiment to end on.
Lilly Stairs: The last thing I wanna say is that, if you are somebody who's going through this, you're struggling with an economic burden, we are here to help.
Whether it's to support you through a clinical trial or to help you, connect you to other resources, we work with a lot of patients who are eager to support other patients and advocates. Let us all be a community that works together.
Aaron Jun: Right, well done. Lilly?
Lilly Stairs: Yes.
Aaron Jun: I don't think anyone's asked you this.
Lilly Stairs: Oh, gosh.
Aaron Jun: What does patient power mean to you?
Lilly Stairs: Oh, no. You didn't tell me you were gonna ask me this. I'm not ready. No, I'm kidding.
Lilly Stairs: Oh, my gosh. It's so interesting because the dynamic is changing. In the doctor-patient relationship, in the patient-payer relationship, in the patient-pharma relationship, patient-centric is a buzzword, but you know what? There are a lot of people who are living it now.
Lilly Stairs: I believe that patient power is you truly owning your health care journey and being able to step up and work with all of these people to initiate change in health care. I'm seeing so many patients who are doing that. I feel like I'm just surrounded by patient power all day. I feel very lucky.

Lilly Stairs: You know what I think? I think patient power is our Breakthrough Crew ambassadors. I really do. They emulate patient power for me. I think that's the best answer I could give you.
Aaron Jun: I think that's a pretty good stopping point.
Lilly Stairs: All right. Well, thanks all so much for joining us!
Next week we'll be back with another patient story, and the week after that, we will bring Aaron back if you like him. Send me your thoughts and if we think he's good enough, we will bring him back.
Aaron Jun: And on this economic burden of disease stuff, we don't want to pretend like this is the only conversation that there is.
If you know anyone who's gone through a journey of their own, if you've gone through anything on your own, if you have resources that you'd like to share, if you would just like to talk to somebody about all this stuff, shoot us a note.
You can find us at aaron@clarahealth.com and lilly@clarahealth.com.
Lilly Stairs: Lilly with two Ls.
Aaron Jun: And Aaron with two As. We'd be happy to
share your story. We'd be happy to maybe have you on.
Aaron Jun: Thanks so much for having me. This was fun.
Lilly Stairs: Yeah, of course. Now we've tried to end this podcast five times, so I'm gonna really end it now.
Aaron Jun: Okay. Bye, everyone.
Lilly Stairs: Bye, everyone.