Hello everyone, and welcome to the, Patients Have Power podcast. I am super excited because today we have Maria Thomas with us, and Maria is a Hyperhidrosis advocate. She does a ton of work in this space. Hyperhidrosis really doesn't have the awareness that it should have, considering how many people are living with it. (You can subscribe to the podcast at Apple Podcasts, or listen to it with the media player above).
I'm going to let Maria tell you all about that, but given that it is November, and it's Hyperhidrosis Awareness month, we're thrilled to have her on the podcast. She's one of our Breakthrough Crew Ambassadors, and she does a lot of incredible work for patients, so Maria, thanks so much for being here today.
Maria Thomas: Hi, thank you for having me.
Lilly Stairs: Of course, so I'd love to just have you, as we start most of our podcasts, give us a five minute overview of your journey as a patient and as an advocate, and perhaps tell us a little bit about hyperhidrosis, because as I mentioned, I think it's something that's not necessarily as well known within the general public.
Maria Thomas: Yeah, definitely. I'll start off with the definition of Hyperhidrosis.
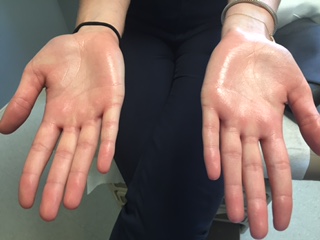
Hyperhidrosis is the medical definition, or medical term for excessive uncontrollable sweating. Approximately five percent of the world's population has Hyperhidrosis, so that's about 365 million people worldwide who are struggling with this.
I've had it since ... First grade is the earliest I remember having symptoms. I had trouble playing Red Rover, or silly childhood games like that because my hands were so sweaty. I couldn't wear Jelly shoes, because my feet sweat so bad that I would slip and slide around in the shoes. When I was about twelve years old, I finally asked my mom, you know, "Why are my hands so sweaty?" So, she took me to our primary care physician, and he prescribed a prescription strength antiperspirant, and told me to apply it at night, and then to wrap my hands and feet in Saran Wrap to help the drug absorb better into my skin.
Maria Thomas: That's not very practical for a twelve year old. That treatment was not effective, and then I just kind of dealt with it over the years. Then when I was a freshman in college, I started just doing my own internet research, and when I was Googling excessive sweating, I did not know that it was actually called Hyperhidrosis. So, through some internet research, I found the International Hyperhidrosis Society. Then at age 30, I became a patient volunteer for one of their Hyperhidrosis symposiums, where they were educating dermatologists on botulin and toxin injections, and just Hyperhidrosis as a disease state in general. I volunteered as a patient, and I got botulin and toxin injections in my hands, and my life really changed from there on out. I left that symposium in Denver that day just feeling like I needed to tell my story, and so I launched my blog that same year, back in 2011, Mylifeasapuddle.com.
Lilly Stairs: I love that name.
Maria Thomas: Thank you.
Lilly Stairs: It is such a cool name. Really, your experience, the way that you tell this story, it's not easy, it sounds like, what you've been through. I think that people might think in their head, "Oh, well it's just sweating." But, that probably impacts a lot of different pieces of components of your life, from dating to sports, to even writing on a test. You know, you're writing, and your hand is creating sweat on the paper.
Maria Thomas: Exactly.
Lilly Stairs: Yeah, so I'd love to just hear, if you could just tell us a little bit more about some of those, maybe challenging experiences that you went through because of your Hyperhidrosis, just in your day-to-day life.
Maria Thomas: Yeah. I think probably the biggest thing is that it can ...
I mean, it affects everything, number one. It affects the clothing that I wear, the activities that I participate in, or not. I'm worried about holding my friend's babies, and either dropping them because I can't get a grip on them, or handing them back soaking wet. My wedding day, I had my Mother in Law sew a towel around the handle of my bouquet, so that I could hold my bouquet properly.
I had a fan facing me at the altar in the church on my wedding day, so that I could feel some air flow because I tend to do a lot better if I can feel air moving across my body. Hyperhidrosis now, as an adult for me, is a downright safety issue because I also have Ulcerative Colitis, or Ulcerative Colitis, however you pronounce it. That's an autoimmune condition, so I have to self inject a biologic medication, twice a month into my stomach. So, if my hands are sweating, and that syringe slips out of my hands, I could lose a precious dose of life saving medication.
Lilly Stairs: Which we all know, and those biologics are not exactly cheap. It's not like an Advil, or you can just get another one.
Maria Thomas: Exactly.
Lilly Stairs: That's not really how it works.
Lilly Stairs: I just can't even imagine. Those are some really difficult experiences to have to go through, and I think it's important that we're bringing this to light, and that you're working to shape this awareness around this condition because everything you just went through, and everything you've just explained, that's hard. That's not easy.
Maria Thomas: It's not, and so you know, a lot of people think, "Oh, you know, it's just a little sweat," and it's not. You know? If you live in a dry world, of course you would tend to think that because you don't understand what it's like. A lot of people don't talk about this condition because it's shame inducing. It's embarrassing, and it makes us feel that we're not worthy of touch. We can develop confidence issues, we can develop social anxiety, body shaming, and negative self-talk. I don't experience all of those things, but I have met people in person who do.
Lilly Stairs: What does the course of treatment look like for Hyperhidrosis?
Maria Thomas: Well, if you picture treatment options as a pyramid, you want to start at the bottom of the pyramid, and work your way to the top because the treatments that are at the top are a lot more serious, and have long-term consequences, and possibly heavy duty side effects. Generally, the first course of action is over-the-counter antiperspirants, and we now have clinical strength antiperspirants, which are still over-the-counter. Then you move into prescription strength antiperspirants. There are oral medications called Anticholinergics that block the acetylcholine in your body, so it blocks your body from starting to sweat. Then up from there, the botulin and toxin injections, iontophoresis, which is when you place your hands and feet into a tray of shallow water, and then you run an electrical current through it. It sounds counter-intuitive to run electricity through water, but that's what happens with iontophoresis.
Maria Thomas: Then, the last treatment option is ETS surgery. That's, Endoscopic thoracic sympathectomy. That's where they go in through each arm pit, and they clamp off individual nerve chains in the sympathetic nervous system. That surgery, while it can be successful for some people, the majority of people I've talked to, and met in person, absolutely regret having that surgery because the compensatory sweating is so severe afterwards. They go in for the ETS surgery to either treat their hands, or their feet, or their underarms, and then they come out with compensatory sweating in their trunk area. So, they're sweating from their chest down to their hips, and they're soaking through multiple layers of clothing. They have to shower multiple times a day, they have to change their clothes multiple times a day, so my one caveat with that surgery is, please do your research on that. Don't just assume that the first page of Google results touting ETS surgery is going to be the best treatment option for you.
Lilly Stairs: Oh, wow. That is a lot. That's a pretty significant list of side effects.
Maria Thomas: Yeah.
Lilly Stairs: Okay. Can I ask, which treatments have you personally tried?
Maria Thomas: I've tried over-the-counter antiperspirants, both regular strength, and clinical strength. I've tried the prescription strength antiperspirants. I've tried anticholinergics, so Glycopyrrolate is a generic name for one of them. I've also tried beta blockers, which a lot of people will be prescribed for anxiety right before public speaking, so a beta blocker helps to lower your heart rate. One of the side effects can be decreased sweating, and it's prescribed as an off-label use. I tried those back in college, and it lowered my blood pressure so much that I just became very lethargic and tired, and I would feel dizzy when I stood up from the classroom in college. So, those were not effective for me.
Maria Thomas: I'm in the process of trying iontophoresis, but it's an interesting feeling when you place your feet in the water, and then turn the machine on. It's kind of like a pins and needles feeling, and my pinky toes tend to tingle a little bit. It's a little bit uncomfortable. It's not painful, it's just uncomfortable for me at the moment, so I'm trying to slowly work myself into that treatment.
Lilly Stairs: Yeah, well who likes pins and needles, right?
Maria Thomas: I know.
Lilly Stairs: Okay, okay. Really, you haven't been able to find, ultimately, something that is keeping it under control?
Maria Thomas: That works long-term, not yet. I have had some success with Carpe Lotion, which is an over-the-counter antiperspirant lotion. It's for your hands and feet, and they also just came out with a new under-arm version. I have some temporary relief with that, which in my book is a success, because if I can have just a few hours of dryness, then that's great for me.
Lilly Stairs: Yeah. Well, it sounds like we need to be doing better in this space with treatments, and I know that you've discussed that you have some background, or experience in looking into some of the clinical trials that are up and coming, or that are currently running. Can you tell us a little bit about what the landscape looks like right now for Hyperhidrosis clinical trials?
Maria Thomas: Yeah. There are definitely companies out there who are paying attention to Hyperhidrosis, and who actually care about this condition. Right now, there's a phase 2 trial right now that's testing the efficacy and the safety of a medication, and then they're going to be moving into Phase 3 trials I believe, hopefully next summer for a topical prescription medication. I know there is another company called Dermira, they just came out with an FDA approved wipe. It's similar to a baby wipe, and it's a topical anticholinergic for underarm sweating, or Axillary Hyperhidrosis.
Lilly Stairs: Okay, so this is good. It sounds like there is some progress being made. There are people working on it, so I'm excited to hear about that. What we'll make sure that we do, in the notes to this podcast, we'll make sure that we include some links to any trials that are currently happening so that anyone who is listening in, and wants to look into, maybe alternative treatment options can check that out.
Editors note: Check out hyperhidrosis clinical trials currently running here.
Maria Thomas: Sounds great.
Lilly Stairs: Knowing that it's Hyperhidrosis Awareness month, what do you want people to know about Hyperhidrosis, and what are you currently doing, or what initiatives are you currently working on this month to help get the word out?
Maria Thomas: I think first, and foremost, if you're listening to this and you think you might have excessive sweating, you are not alone. Please, come to my blog because my stories are your stories. Right now for the month of November, the overall theme of Hyperhidrosis Awareness month is, use your voice, and so I've partnered with the International Hyperhidrosis Society. I'm helping them with some of their content during the month of November. They're also doing an amazing campaign where you can submit your story, your sweat story, and have a chance to be archived in the library of Congress, which is really amazing.
Lilly Stairs: Oh, wow.
Maria Thomas: I encourage people to go to that website as well, Sweathealth.org, and you can submit your story there.
Then personally, on my own blog, in the last three months, I've opened it up to other people's sweaty stories. I have Jess's story, she's a five year old who lives in the United Kingdom. I have Martin, who lives in Kenya. I have Carrie from Ohio, and I have Leanne from Ontario. Then next month, you'll meet another woman who is from the Philippines. It's been really neat to be able to connect with people all over the world, and let them know that they're not alone, and that there is nothing to be ashamed of.
You know, it's not our fault that we have Hyperhidrosis, and so I think you can find a lot of strength if you have the courage to speak up and use your voice.
Lilly Stairs: That is so incredible. That is a wide range of countries and people you've been able to reach. What's been most interesting to you, talking to so many different people from different cultures and backgrounds, what's been the most interesting as you've had conversations with all of them?
Maria Thomas: I think ... There's a quote from CS Louis, and it's something to the effect of, "Friendship is born at that moment when one person says, you too, I thought I was the only one." Just being able to make that connection. People have said, "I am so glad that I found you. I was Googling Hyperhidrosis and shoes," or, "I was looking for some sandals that I can wear in the summer even though my feet are horribly sweaty," and they find my blog because I've written just about everything. Every story you can think of is basically on my blog, so just being able to connect with other people because I think there's strength in connections.

Lilly Stairs: Absolutely, and I'm going to pry a little bit there, and just ask you, what do you think is the most personal story that you've shared on your blog, and why was it important to you to share that with others?
Maria Thomas: I would say the most vulnerable post on my blog is about groin sweating, because that's a thing. Hyperhidrosis does not discriminate, so some people have sweating in their groin area. It's something that needs to be talked about. There is an entire isle in the grocery store dedicated to antiperspirants, and body powders, and body sprays. You know, panty liners, and all that crazy stuff, so clearly, I'm not the only one that experiences that. I think that's probably the most vulnerable post.
Lilly Stairs: Well, of course. When you're looking at some of these different treatments that are coming out, are there any treatments that exist for the groin sweating, or not really at this point outside of the over-the-counter?
Maria Thomas: Not really at this point. I'm sure there could be room for an off label use for Cubrexa possibly, because that's a topical, and it's in a wipe form, so you could definitely wipe it on the sides of your legs, hopefully. I'm not advocating that at the moment. It's a brand new medication that was FDA approved, so there's still time, and testing, and prescribing that needs to happen before we can get there.
Lilly Stairs: Yeah. Well, thank you for your willingness to share that because I know that when it comes to some of these more personal, or what some people would consider more "embarrassing", you know, it's something that we need to talk about. There are a lot of people who are experiencing, whether it be Hyperhidrosis, or a lot of other stigmatized conditions, that it's people like you, when you come out and talk about it, it makes all the difference because people feel less alone. It's kind of like you were talking about, that friendship is born in that moment of, "Oh, me too."
Maria Thomas: Yeah.
Lilly Stairs: Another piece I wanted to go back to here, you briefly mentioned that you also are living with ulcerative colitis. I know that we have a lot of listeners who are in the IBD space, and we actually also have IBD Awareness week coming up the first week of December. I was just curious to know what your experience has been like, living with the ulcerative colitis, alongside the Hyperhidrosis.
Maria Thomas: Yeah. It's been difficult. I experienced the worst flare of my life ... Well, let me back up for a second. I was diagnosed at age 34. I went through some oral prescription medications, and was under control, and then I moved out of state. Just kind of, the perfect storm, and I had as really bad flare, back in 2016. At that point, I became hospitalized for Easter weekend. Timing was impeccable, really. Easter weekend, the GI doctor comes in. I had already been scheduled for a colonoscopy, so I was ragingly sick, could not control my bowels. Then in the hospital, I still had to do the big jug of prep to go in for the colonoscopy, and I came out of that procedure, and the GI doctor said, "You have a raging case of UC, and we need to put you on Humira, which is a biologic injectable medication."
Maria Thomas: I was really kind of at the end of my rope treatment wise, but not once did any one of my GI doctors in Texas, or in Colorado at the time, they never said, you know, "Gosh, you might want to avoid Gluten, or grains in general. You may want to avoid sugar. You need to clean up your gut health." I had to go to a functional medicine doctor and spend about 1200 dollars out of pocket to really get a handle on my condition.
I think being your own best health advocate is really important, no matter what type of condition or disease you might have.
Even when I was in the hospital, I was having to tell the nurses, "No, I can't eat that because I'm supposed to be going in for a colonoscopy, and I can't have red jello because you can't eat red dye when you have a colonoscopy." Stuff like that, that you would think should be in my chart, was not in my chart.
Lilly Stairs: Isn't that unbelievable? Every time I hear that doctors are not talking about diet, especially when it comes to a disease of the gastrointestinal tract, I'm always shocked. It is really a shame that a lot of these functional medicine, nutrition, any of that type of care is not always covered by insurance. Like you said, you had to go out of pocket. We've started to see more clinical trials in the space of diet and lifestyle changes because it really makes sense that that would go hand-in-hand with medication. I applaud you for being your own advocate, and trying to get everything under control. Out of curiosity, did you find that diet helped your Hyperhidrosis at all, or not really?
Maria Thomas: No. I wish. I've tried everything in the book to treat my Hyperhidrosis. I've heard things like, "Oh, take Sage tablets, or drink Sage tea, and don't drink water, and just dehydrate yourself." Just crazy stuff, but no, diet hasn't made a change at all in my sweating.
Lilly Stairs: Okay. As you look at ... With these two, has it been difficult for you, because it sounds like Hyperhidrosis, you've had for a long time, a lot longer than the UC. How do you feel about the difference in awareness between Hyperhidrosis and UC? Because it sounds like both of them have affected your life on a very serious level.
Maria Thomas: Yeah. I think there's definitely more awareness around IBD, and UC specifically. How often do we see the commercials on TV for Humira, or Entivio, or any other new medications, or newer medications to the market place? We're finally starting to see commercials now for Hyperhidrosis, which I think is great, but I think it's also important too, that when people hear the word Hyperhidrosis, that does not automatically mean excessive underarm sweating. People can have Hyperhidrosis in their hands, their feet, their groin. They can have craniofacial Hyperhidrosis, where they're sweating from their head, or their face. In some severe cases, people can have all-over body sweating. Hyperhidrosis does not just mean underarm sweating.
Lilly Stairs: So fascinating. I feel like I've learned so much from you in the course of this podcast. I know that our listeners are going to get a lot out of it. Undoubtedly, either they themselves are living with Hyperhidrosis, or someone they know probably is, given those numbers that you shared at the beginning of the podcast. I so appreciate you sharing all of this insight and wisdom. I, of course, have to end our podcast by asking you what, Patients Have Power, means to you.
Maria Thomas:
Patients Have Power is really kind of a guide post for everyone out there who is suffering in silence. You are the expert on your body, and so you can take your power back, and be your own best health advocate. Don't be afraid to speak up.
Lilly Stairs: I think you are just an absolute shining example of Patients Have Power, and I'm so thankful that we have the opportunity to work with you as a Breakthrough Crew Ambassador, and I'm thankful to all of the work that you're doing in the Hyperhidrosis space because it's much needed. I think it's important that we all continue to work to shine light on some of these diseases that maybe haven't gotten the attention that they need. We need to give all ... We should be trying to give attention to diseases across the board because that's how we get stronger awareness, and funding for research, and support to those who need it most. I applaud your efforts, and I encourage everybody to check out Maria's blog, My Life is A Puddle. Get in touch with her if you have any questions. Thank you again, for joining us, Maria.
Maria Thomas: Thank you, and I just wanted to mention one other thing, in December, if you go to the Pharmacy Times, continuing education website, you might just find a Hyperhidrosis continuing medical education activity, and you might also just find a video with me in it.
Lilly Stairs: Oh, fun. Alright, well we'll be sure to check that out.
Maria Thomas: I'm very excited.
Lilly Stairs: We'll make sure that we linked that as well in the show notes. Thanks everybody, looking forward to seeing you again next week.