Hey everyone! Thanks for tuning in to our Patients Have Power podcast. I'm Lilly Stairs, your host and Head of Patient Advocacy here at Clara Health.
Our latest Patients Have Power episode is called "Ya can't teach compassion." (You can subscribe to the podcast at Apple Podcasts, or listen to it with the media player above).
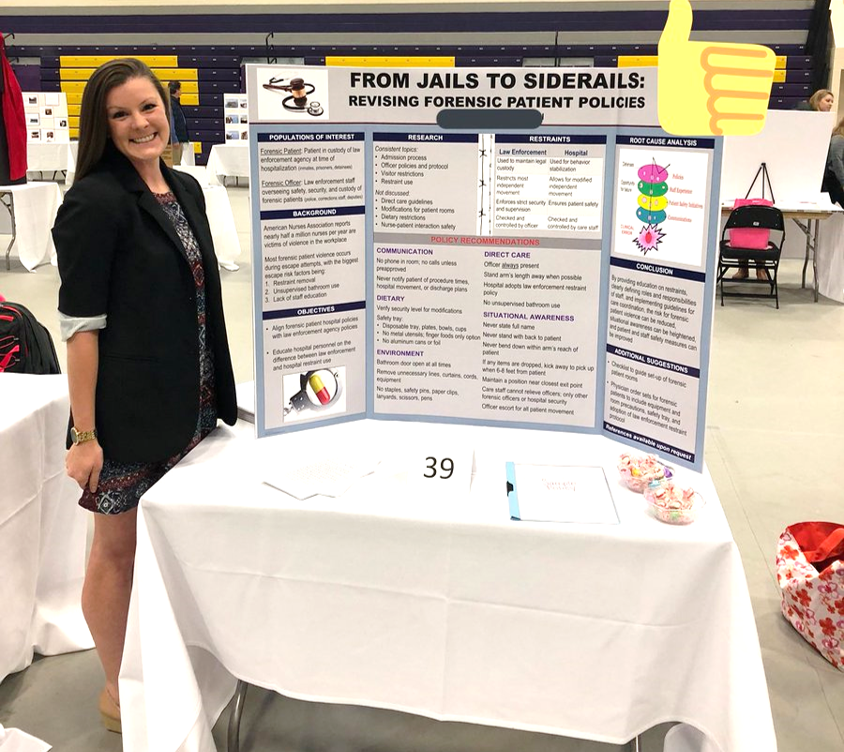
In this episode, I had the absolute best time interviewing our first ever nurse on the podcast, Amber, also known as Wheezy Nurse on social media. She is the nurse that we all want to have when we're in the hospital. She's the nurse who does whatever it takes to make you feel comfortable and ensure that you are empowered and look up to her in everything she does for patients. And of course, had an absolute ball interviewing her because the girl is hilarious.
Amber and I chat about she focuses on the patient experience in her work as a nurse. Ya can't teach compassion, but maybe we can teach patient empowerment to everyone in healthcare!
Below is a transcript of the episode for your reading pleasure!

Lilly Stairs: Hi everyone! Today we have the amazing Amber, better known as Wheezy Nurse on Twitter.
We're very lucky to have her here. I would call her a Twitter celeb for sure. And what's really exciting is that Amber is actually our first guest who is not a patient, but actually a nurse! She really champions the patient experience by making sure that patients are empowered through their journey.
I have been so impressed by Amber really as ... she's over here...
Amber Lynn: I'm blushing!
Lilly Stairs: I don't think I've ever seen a nurse who has such passion and a drive to really be by the bedside and make sure that patients feel supported. I wish that you were my nurse. I wish that you could be everybody's nurse. We just need to clone you someday.
Lilly Stairs: So anyways, enough of me talking. I really just want to jump into talking with you about your journey.
How did you end up as a nurse and how have you made all of these decisions to really ... I think so much of what you do wasn't necessarily what you were taught. It's just almost, it's like a gut instinct for you. It's like it's something you want to do.
So I'd love for you to just dive in and tell me a little bit about that.
Amber Lynn: Sure! My background is:
- I went to college in the greater Boston area.
- I graduated in 2013, with my Bachelor's
- I'm actually back in school now for my Master's with a focus in clinical nurse leadership - so I actually hope to focus on bettering the patient experience. That is and always has been my passion.
I am a big proponent of hourly roundings, spending more time at the beside, getting to know your patients, because if you build you a better nurse patient rapport and a better relationship with your patients you're going to get a better assessment. They're going to feel more comfortable talking to you. They're going to feel more comfortable giving you actual facts of their history.
Sometimes people brush over really important facts when they're coming into the hospital. "Oh, well you know what? I'm coming in with a facial droop, but I don't need to tell them that I like to hike." Well, are you around ticks? Are you thinking that this isn't a stroke and that it's maybe a Bell's palsy, or something from lime disease instead?

You never know, and there's a lot of facts you can actually learn from your patients that would be pertinent to their medical history and their prognosis just by talking to them and making them feel more comfortable talking with you. So that is something that I hope to focus on throughout.
Amber Lynn: As far as my education, anyone can be taught and anyone can learn clinical skills, but you can't teach compassion. It's just something you either have or you don't. And I like to think that I have it.
Lilly Stairs: Oh, I think so!
Amber Lynn: But I will take five more minutes to hold the patient's hand while they cry instead of running off and sitting down to chart. If it takes me a few more minutes at the end of my shift to document, fine, but I'm not leaving until my patient is comfortable.
Lilly Stairs: Wow. And how do you, with the time demands? I mean, we're constantly hearing about, and patients and caregivers are talking about, and physicians and nurses for that matter, the crazy time constraints there are, and the pressure that is being put on the healthcare system. How do you manage that?
How do you give the extra time to patients when there's so much to be done? And there is, often I know nurses and doctors have these big caseloads.
Amber Lynn: Yup. So, one thing that my hospital is currently trying to do is solidify nurse patient ratios.
It's something that's coming up on ballots now nationwide to make sure that nurses aren't getting burnt out. That they are giving adequate and appropriate care to their patients, and can actually fit everything within these time allotments.
So right now, we're focusing on four to one ratios. So four patients to one nurse. It doesn't always happen, but I've gotten to a point where I know how long it can take me to document. I don't need to do it at the beginning of my shift. I don't need to do it right away. And half the time I break up my assessments. I'm not going to wake someone up at 7:00 o'clock in the morning and do a full head to toe assessment. "Hey, turn around so I can see your butt and see how your skins looking!"
No, I'll wait until you get up till you go to the bathroom and then I'll take a little peek at your butt and make sure your skin is good.

Lilly Stairs: Thank you for saying that. I, you know, I remember when I was in the hospital, they would wake me at 5:00 o'clock.
And sleep was the only time that I felt like I had solace and I could finally be taken away from the pain, but then they would wake me up at five in the morning to do all these things and I'm like, "Could you please just let me sleep? This is the only time that I have where I'm not in pain."
Amber Lynn: Yup.
Lilly Stairs: And so you have found a way to let patients be more comfortable.
Amber Lynn: Yup. So, little by little I'll do my assessments. A lot of people like to do everything up front and document, get everything in order and then they can take the rest of the shift as they will. I will do everything little by little.
So, I'll pend all of my assessments. I'll throw in a few more facts here and there throughout my shift rather than sitting down and just doing them all. I think with that, it gives me more time throughout my shift to look at my watch and say, "You know what? It's almost right on the hour. I'm going to go around and check in."
Every hour, I make sure that I'm going into a patient's room or at least standing by the door waving and saying, "Are you all set? Is there anything you need?" It ensures continuity of care, makes the patients feel more comfortable. They trust you because you're reliable.
I think that makes a difference.
Lilly Stairs: Wow.
Amber Lynn: It's simple.
Lilly Stairs: I just want to blast this through every hospital everywhere around the world. This is just incredible.
Lilly Stairs: And there's actually something I wanted to make sure that we capture on here that you talked about during the, What the Fix (#WTFix) Twitter chat, which is something you do with post-it notes. Do you want to share a little bit more on that?
Amber Lynn: Sure. When I was first starting within nursing, I was doing the evening shift, so three to 11. By the time I give report, by the time I'm about to leave, it's 11:30, 11:45 at night.
Most of my patients were sleeping, so I would build up this good rapport with patients, and if I wasn't coming back the next day or even if I was, I would leave them a little note. They'd be fast asleep. I'd put just a tiny little:
"It was great getting to know you. I wish you nothing but the best. Good luck with your journey. Heart. Nurse Amber."

And it would be on their menu so when they woke up the next day to order breakfast they would see it and all I wanted was, "Oh, she was thinking of me." That's it.
But then it turned into every single patient I had I was doing it. And I had family members writing notes back and forth with me even if I didn't see them. They would put them on the boards. "Thank you so much for thinking of us." "Thank you for taking time to make my family member feel comforted."
It's the little things that matter the most. Healthcare has turned into a hurry up and wait system. You hurry up and get to the ED and then you're waiting to be seen. You're waiting for the test results. You're waiting for a test to even be done.
Amber Lynn: So, nursing, we're capturing all of that. We're seeing you as you're waiting. And there's not much we can do. A lot of times it's the radiologist that has to read a report. It's the doctors that need to come around and round on you and give you an update. Caseworkers are trying to find rehab placements - and what am I doing?
I'm the one that sees you. So, cha cha cha, let me do a little dance! Let me sing for you! Let me do something to make this waiting game into a good experience.
Lilly Stairs: Amber, we're going to send you on the road to do a show and just ... You are so captivating! Everything you say is just so on point and I know, I'm sure for many of the patients listening and healthcare providers listening, those who truly care about the patient experience are sitting in their seats and going, "Yes! This is awesome!"
Amber Lynn: Yes girl, yes!
Lilly Stairs: And that just made me think of giphys? jiffys? Which one do you say?
Amber Lynn: The giphys. I say gifs. I don't know.
Lilly Stairs: This is a really hotly debated topic. And I won't get into it now. I get told giphy/jiffy all the time and people feel really passionately about it.
Editor's note: Officially, Clara Health endorses the giphy pronunciation.
Lilly Stairs: The reason I'm transitioning there is because I want to talk to you a little bit about Twitter and how you just blew up on Twitter. How did you even get on Twitter? And then get started with it? And what's it been like to now have what, are you almost at 50,000 followers?
Amber Lynn: Yeah, I think I'm just shy of 50,000. I first started on Twitter in 2013 once I graduated from nursing school, and I kind of started as a way to vent about how much I hated studying and how much I was just hating the limbo after graduating.
That awkward time where I'm not a nurse yet. I have my degree, but I need to take my exam and I'm sort of unemployed and I don't know what to do with my life. I'm just a lost puppy.

Amber Lynn: I started this account and it originally started out as Asmatic Nurser, something like that. Actually I think it was WheezyLBaby, like Wheezy F Baby, Lil Wayne.
So I started out with this completely different person, but I was venting. I was including different fun facts as I was studying, different ways that I remember material, fun study tips and I would just harass people.
I would just like every single tweet that they'd be posting. I replied to everyone and I've only got like 30 followers. And they're like, "Who is this girl? What is she doing?"
Amber Lynn: So I started following tons of people and trying to study at the same time. Just posting fun little clips here and there. Then Twitter started building.
I found these different people that were passionate about the same things that I was. Whether it was fun ways to study, or nursing humor. Then I would follow these people. We'd go back and forth, and then I started to gain a little more of a following.
Amber Lynn: Once I became a nurse, my patient stories really hit home with a lot of people. So, once again, started building.
And I think the cusp of everything, where I really started to gain a following was when Stat News, the medical subset from the Boston Globe, kind of shouted me out as top 13 clinicians to follow on Twitter.
Amber Lynn: You've got these huge people, and then you've got Wheezy Nurse. "Hey guys, what's up?" You're all like really cool people and authors of books and I'm just me being weird in the corner.

Amber Lynn: So after that, it kind of boosted me up a little bit, and then I started getting really, really passionate about patient advocacy and patient outcomes, the patient experience.
I started reaching out to different companies, and I made these invaluable connections with people like you and with HealthSparq, which is a company out in Portland, Oregon that focuses on the patient experience and patient empowerment as well.
Amber Lynn: Honestly I never thought Twitter would get this far. I was just happy that my mom thought I was funny. Now I'm close to 50,000 people think I'm funny so I guess I'm funny.
Lilly Stairs: Well you are. Not only are you funny, but you also have this inspiration. It's really special to be able to carry being both a comedian and being inspirational. I don't often see those two paired together.
Lilly Stairs: So do you feel like you're making an impact in helping other nurses with the work that they're doing, and helping them become more patient centric via your work on Twitter?
Amber Lynn: Yes. I think even in real life as well now that I've become a more experienced nurse.
I just started clinical instructing and one of the first things I told my students was to bring post-it notes because I want to see the fun facts that they learn about their patients.
Amber Lynn: We walked through and I didn't even say a patient's name once and I said, "So, this patient in this room has a 20 year old cat, and the only way that she can get hydration is through a little IV boluses that they give her once a day." And they're like, "How in the heck do you know that?"
'Cause I talk to my patients.
Because I learn fun facts about them every day and that's what your post-it notes are for. That's what you're going to do.
I want you to write one fun, interesting fact about every single patient that you have and bring it back to me because I guarantee it's gonna make a better relationship with that patient.
Lilly Stairs: Amazing.
Amber Lynn: So even just the impact that I can have over five students during a semester is worth it. Never mind 50,000 people.
Amber Lynn: Absolutely. So you're making changes everywhere. It's awesome. It's awesome. Online, in person.
Amber Lynn: Changing the world, yeah!
Lilly Stairs: You're doing all this online advocacy, you're teaching, you're a nurse. I really don't know how you, you work with all these companies.I don't really know how you keep up with all of it.
Lilly Stairs: And I do want to take a moment to talk a little bit about clinical trials as well.
Amber Lynn: Sure.
Lilly Stairs: Given that we've been doing some work together on this. I'm trying to figure out how exactly we talk about clinical trials, and what the nurse's role is with clinical trials.
And I'd be curious to know what education, if any, nurses are really given in clinical trials, and what the rules are around being able to talk about that within the hospital and with patients because as we've discussed. A lot of it's that we want patients to be empowered with the knowledge that they are treatment option. But it's often not discussed. And so that's a big part of the problem.
So if you could just talk a little bit about that from the nurse's perspective I think that would be really, really fascinating for our listeners.
Amber Lynn: Within nursing school, there's an overwhelmingly large amount of knowledge that we need to conceptualize and then critically put into practice. So a lot of the focus is more on the fundamentals of nursing rather than patient options.
Once you start working within the medical setting, depending on where you're working. Whether it's in a clinic or the hospital, there's different specialties and then there's always options. With nursing, it's very tough because you don't want to sway a patient in the direction of something that is maybe not best for them.
So you need to give them enough information to make the best decision for themselves.
Lilly Stairs: Yup.
Amber Lynn: I will never sway my patients in the direction that I want them to go in. I encourage the doctors to do the same.
Give patients options rather than telling them they need to do something. Just giving them the power over their own decision making and being able to really give them all the knowledge that they would need to make an informed decision. So from nursing, that's what we do. We can educate. That's one of the biggest things that we can do.
Just educate.
Give you the knowledge that you need to make the best decisions for yourself and for your treatment options.
Lilly Stairs: What I think is interesting, and I'd be curious to know if you agree, when we're talking about how nurses really are the ones who are by the bedside the most. You're doing your job right? You're by the bedside most.
So you're getting to know the patient on a more intimate level than the physician is, most likely. So are you able to address, are you able to have conversations around educating when it comes to treatment options, or is that off the table? I'm not even sure legality wise.
Can you talk about those options and have an open conversation with them?
Amber Lynn: We can have open conversations if it's something a patient feels passionate about. I usually ask what are the patient's specific goals. Usually, physician goals are different from patient goals. There's a lot of people that have gotten into the mindset of the old school way of thinking. "The doctor said I need to do this so I need to do it. Well the doctor said that this was the best option for me, so I have to listen to the doctor."
No, you don't have to. What is your goal? 'Cause the doctor's goal is to either eradicate this disease or ship you off to the next session that will give you more physical therapy, whatever it is.
A lot of times their goals do not coincide with the patient goals.

Amber Lynn: So as nurses, I think the biggest thing we can do is listen to the patient about what their specific goal is. If a patient came in with a stroke and they're only goal is to walk, then maybe we need to focus on more physical therapy and mobility options.
If someone wants to see their youngest daughter graduate college, maybe they want to go through a clinical trial to find the best treatment option for their cancer.
Whatever it might be you need to listen to the patient about what their goals are in order to then tailor their education and treatment options.
Lilly Stairs: I love it. I love it. I could listen to you talk all day.
Is there anything that you recommend for, having worked with so many patients day to day and really getting to know patients, what do you recommend to our patient listeners out there when they're in the hospital to help them feel empowered?
Because often times when you're in a hospital bed it's not really a place where you are really given the strength to feel empowered, right?
Amber Lynn: Yeah.
Lilly Stairs: So what are your tips for patients to feel empowered and really make sure their voice is being heard when they are in the hospital?
Amber Lynn: I would recommend taking notes. If you are in the hospital and you're able to have a caregiver or an advocate with you, whether it be a family member, friend, have them take notes as well. A lot of times you'll pick up on things that an outside perspective won't.
So, if you have two people taking notes when the doctors are in the room doing rounds you can then look back and see what questions you might have. By having a record of everything that has been discussed, you can then feel empowered to ask the questions that you might have forgotten to say or questions after reviewing the information you received.
)
Amber Lynn: I think asking questions and not being afraid to request a second opinion is big.
Lilly Stairs: Yeah.
Amber Lynn: A lot of times if you're in a medical system because of your insurance or what have you, it might be a team of doctors that you've had for 20 years. And although you might trust them, you might want a second opinion. And second opinions are fine. Doctors are okay with that.
Lilly Stairs: They are. I think that's actually something that a lot of patients, I know I've felt it, and I've talked with other patients who have been like, "I feel uncomfortable because I have this standing relationship with my doctor and I don't want them to feel like I don't trust them, but I also need to do this for myself."
Amber Lynn: Mm-hmm (affirmative). Yup. Exactly.
Lilly Stairs: So how do you recommend approaching that conversation?
Amber Lynn: I would always preface it as,
"You've been with me throughout my journey and I value your opinion so much, but to make sure that this is the right decision for me and my future, I would love to get a second opinion to then put in a different mindset in relation to my care.
So, I value your opinion. I value your plans of care, but I would love to get a fresh set of eyes to look over my case and even just instill that this the right decision for me."
Lilly Stairs: Yeah. I love it. Wow, we have just covered so many topics in this 20 minute podcast that I'm so excited about everything we've discussed and I want to bring you back to have more conversations.
Amber Lynn: I am so willing to do that.
Lilly Stairs: Yay! I do have one more question I want to ask you before we wrap up.
Amber Lynn: Sure.
Lilly Stairs: What does "patients have power" mean to you?
Amber Lynn: Patients have power is probably one of the best little catch phrases so I don't know if you guys came up with it or if I came up with it, but I'm just saying I use it all the time anyway.
Lilly Stairs: We did! I love it.
Amber Lynn: Patients have power in every aspect of healthcare. They have power over their choices, their decisions, their treatment, but patients are strong and I don't think that a lot of people realize that.
You might feel weak when you're in the hospital bed or you might feel helpless when you don't know what to do about your treatment options, but everyone has so much inner strength. And there's endless possibilities for everyone.
Lilly Stairs: What a brilliant answer. Well, thank you so much for joining us today, Amber.
Amber Lynn: Of course.
Lilly Stairs: It was such a pleasure to have you. We will definitely be having you back. I highly encourage everyone to follow Amber on Twitter, Wheezy Nurse. And you're on Instagram now too, right?
Amber Lynn: I released my personal Instagram! It's @AmberSushiii. S-U-S-H-I-I-I.

Lilly Stairs: So, if you want to get to know Amber personally like she gets to know her patients, head over to Instagram. And thank you all so much for joining and we look forward seeing you in a few weeks.
Thank you all so much for joining us. We'll see you in two weeks for our next installment. In the meantime, be well and remember that you hold the power.
If you aren't already, be sure to follow Amber on Twitter under @WheezyNurse, Instagram @AmberSushiii, and definitely check out her YouTube page where she does Wheezy Wednesdays!